What is Crohn’s disease?
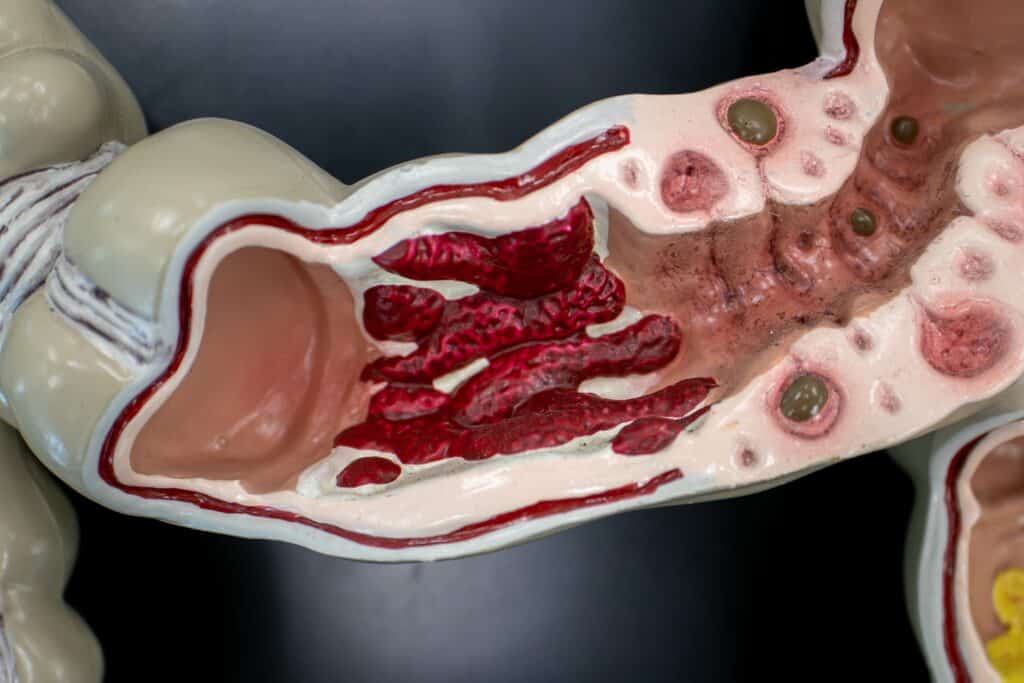
Crohn’s disease is an incurable inflammatory disorder that can affect any part of the gastrointestinal tract. The gastrointestinal tract is a system of body organs responsible for carrying and digesting food, absorbing nutrients, and getting rid of waste. Inflammation (red, swollen, and tender areas) always affects the innermost lining of the gastrointestinal tract, called the mucosa. However, the disease can affect the deeper layers of the gastrointestinal wall and even extend through the entire bowel wall. The exact cause of Crohn’s disease is unknown. Current research is exploring the possible connection of the disease to immune system problems and bacterial infections.

What are typical symptoms of Crohn’s disease?
Crohn’s disease can present as abdominal disease, anorectal (anus and rectum) disease, or both. Patients with Crohn’s disease are at greater risk of developing a fistula. A fistula is a small tunnel that tracks from one portion of bowel to either another portion of bowel, another organ, or the skin. Symptoms vary widely among patients and often come and go over a long period of time.
Possible symptoms include:
How is Crohn’s disease diagnosed?
Crohn’s disease is typically diagnosed and treated by gastroenterologists (GI doctors), but your first encounter with a doctor regarding your issues may be with a colon and rectal surgeon. During the first visit, your colon and rectal surgeon will perform a thorough medical history and physical exam. To aid in diagnosis, they may also examine the inside of the bowel using a flexible instrument with a lighted camera. X-ray studies and laboratory tests such as stool samples and blood tests may also be done. This evaluation will provide information on the extent of disease and help guide treatment.
How is Crohn’s disease treated?

Post-treatment Prognosis
It is important to follow up with your physicians so they can devise an ongoing management plan to control your symptoms. When you have Crohn’s disease, you must stay on medication throughout your entire life. Crohn’s that impacts the colon (large intestine) increases your risk of colon cancer. This risk goes up after 8 to 10 years of ongoing colon involvement. For those patients, it is key to undergo regular follow-up colonoscopies (examination of the colon using a flexible instrument with a lighted camera).
How can I reduce my risk of recurrence?
Recurrence is most common in patients who stop taking their medications, so it is vital to follow your physician’s orders. Smoking negatively impacts every organ in the body and presents health risks for everyone, so quitting is advised. For patients with Crohn’s disease, smoking has been linked to higher recurrence rates, so quitting can reduce this risk.
What is ulcerative colitis?
Ulcerative colitis (UC) is an inflammatory disease affecting the large bowel (colon and rectum). In UC, the inflammation is confined to the internal lining of the intestinal wall (mucosa). Medical management is typically the first option for treatment. UC can go into remission and recur (come and go). If surgery is needed for UC, it is usually curative. The exact cause of UC is unknown, but it is not contagious. Potential causes include immune system abnormalities and bacterial infection.
Is there anything that increases my risk of ulcerative colitis?
Men and women are affected equally and people of all ages can develop UC. A family history of UC slightly increases the risk of the disease.
What are the symptoms of ulcerative colitis?
Most patients develop symptoms in their 30s. A smaller number experience symptoms for the first time later in life (ages 60 to 70). The symptoms of UC are similar to another inflammatory bowel disease, Crohn’s disease. UC, however, only affects the colon and rectum.
The most common symptoms of UC include:
How is ulcerative colitis diagnosed?
Ulcerative colitis should be diagnosed by your doctor. Often, a colonoscopy is performed to diagnose UC. A colonoscopy looks at the inside of your colon and rectum to find ulcers and inflammation characteristic of UC. This evaluation helps determine the extent and severity of UC, rules out other diseases such as Crohn’s disease, and guides management. Additional testing may include blood tests, stool samples or imaging such as CT scans or X rays.
How is ulcerative colitis treated?
Postsurgical Prognosis
After surgery, five to six bowel movements a day and one at night can be expected with a J pouch, maybe even more. Medications can be used to decrease this. Some patients may experience leakage or incontinence (inability to control bowel movements). Infection or inflammation may develop in the pouch. This can be treated effectively with antibiotics or steroids. Due to complications, about 10% of pouches must be removed and a permanent ileostomy created.
Long Term Follow-Up
Regular follow-up medical appointments are scheduled. During these periodic visits, your physician will evaluate the function and health of the pouch.