What is a colonoscopy?
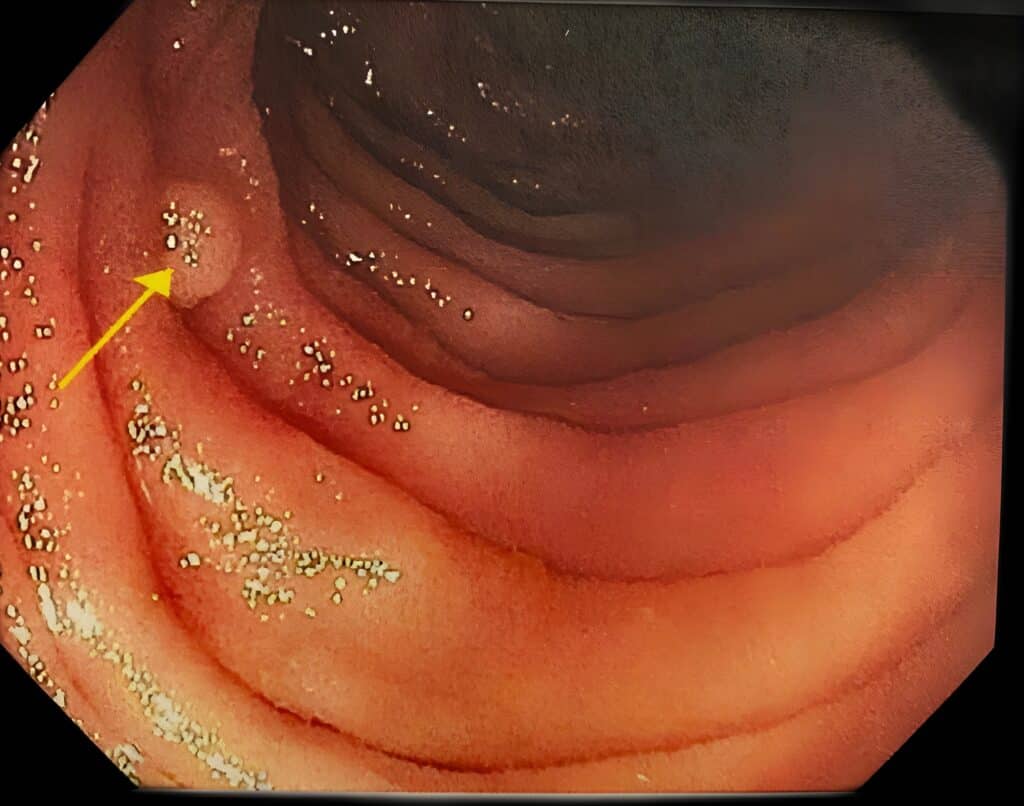
Colonoscopy is an effective procedure to diagnose abnormalities of the large intestine and to screen for colorectal cancer and colorectal polyps. A colonoscope is a long, thin flexible instrument that provides magnified views of the colon and rectum. The procedure is frequently performed in an outpatient setting with minimal discomfort and inconvenience. Because colonoscopy allows doctors to identify and remove certain types of colon polyps that may develop into cancer, colonoscopy can be a therapeutic and even life-saving procedure.
Who should have a colonoscopy?
Screening refers to the process of examining otherwise healthy patients in an effort to detect previously undiagnosed colon polyps or cancer. The goal of a screening program is to detect disease at its earliest stages to allow for successful treatment. As part of a colorectal cancer screening program, colonoscopy is routinely recommended to adults starting at age 45. Patients who have a family history of colon or rectal cancer or polyps may be recommended for a colonoscopy earlier and more frequently than those without a family history of cancer. Your doctor may also recommend a colonoscopy to evaluate symptoms such as rectal bleeding, a change in bowel habits, or unexplained abdominal pains.
Colonoscopy may also be recommended for:
Who can perform a colonoscopy?
A colonoscopy is performed by experienced physicians who are specially trained in this type of procedure. Typically, colonoscopy is performed by gastroenterologists, colorectal surgeons, or general surgeons.
How is a colonoscopy performed?
One or two days prior to the procedure, most patients must complete a bowel “prep”- a prescribed preparation consisting of liquids and/or pills or enema that will cleanse the bowels of stool and other residue. This allows for complete visualization of the bowel surface during the procedure. Your team at Sacramento Colon & Rectal Surgery Medical Group will give you a list of dietary and medication restrictions to adhere to in the days leading up to the procedure. The most important part of the procedure is your completion of the cleansing process as requested by your physician. If you have any questions at all, do not hesitate to discuss your concerns with your physician before the day of the procedure.
During the colonoscopy, most patients receive intravenous sedation. One or more medications are administered to help patients remain comfortable for the duration of the procedure. The colonoscope is inserted via the rectum and advanced to the first portion of the colon, where it is connected to the end of the small intestine. Any polyps or other abnormalities encountered during the colonoscopy will be removed and/or biopsied and sent for analysis.

For most patients, the entire procedure takes less than an hour. After the colonoscopy is completed some patients may experience slight discomfort in the form of abdominal cramping and “gas pains,” though this quickly resolves by passing any gas/air that was pumped into your colon during the procedure. In many cases, patients do not recall specifics of the procedure itself due to the sedation. It is always important to have the individual who will be taking you home be there to discuss the discharge instructions with the physician and nurse before discharge.
Following a colonoscopy, patients usually resume their regular diet. Resumption of your preprocedure medications will be determined by your physician. Some restrictions for driving and activity levels apply when intravenous sedation medications are given to sedate patients immediately prior to colonoscopy. These medications affect judgment and coordination for variable amounts of time following the procedure. Most patients are able to resume normal activity the morning following the colonoscopy.
What are the benefits of colonoscopy?
Colonoscopy is the recommended means of colorectal cancer screening. The procedure allows for detection and removal of colon polyps that are prone to transform into cancer. Also colonoscopy is used for investigation and diagnosis of other diseases that affect the intestines and present with a variety of symptoms.
What are the risks of colonoscopy?
Colonoscopy is a very safe procedure with few complications, occurring in less than 1% of patients. Infrequent risks include bleeding, perforation (a tear in the intestine), rare side effects from sedation medicines, and inability to visualize the entire colon for polyps or other conditions. For anatomical reasons your physician may deem it unsafe to complete the colonoscopy and your physician will therefore terminate the examination. In such instances, your physician will discuss with you whether or not additional or alternative examinations are indicated.