At Sacramento Colon and Rectal Surgery Medical Group, the experienced physicians specialize in the surgical treatment of anal fistulas that cause pain or other symptoms. The providers can also create treatment plans to prevent future abscesses and fistulas. Call the office in Sacramento or Roseville, California, to schedule a visit or book an appointment online today.
What is an anal fistula?
An anal fistula (also commonly called fistula-in-ano) is frequently the result of a previous or current anal abscess. This occurs in up to 50% of patients with abscesses. An anal fistula is a tunnel that connects a clogged gland inside the anal canal to the outside skin. It frequently goes through the anal sphincter muscle.
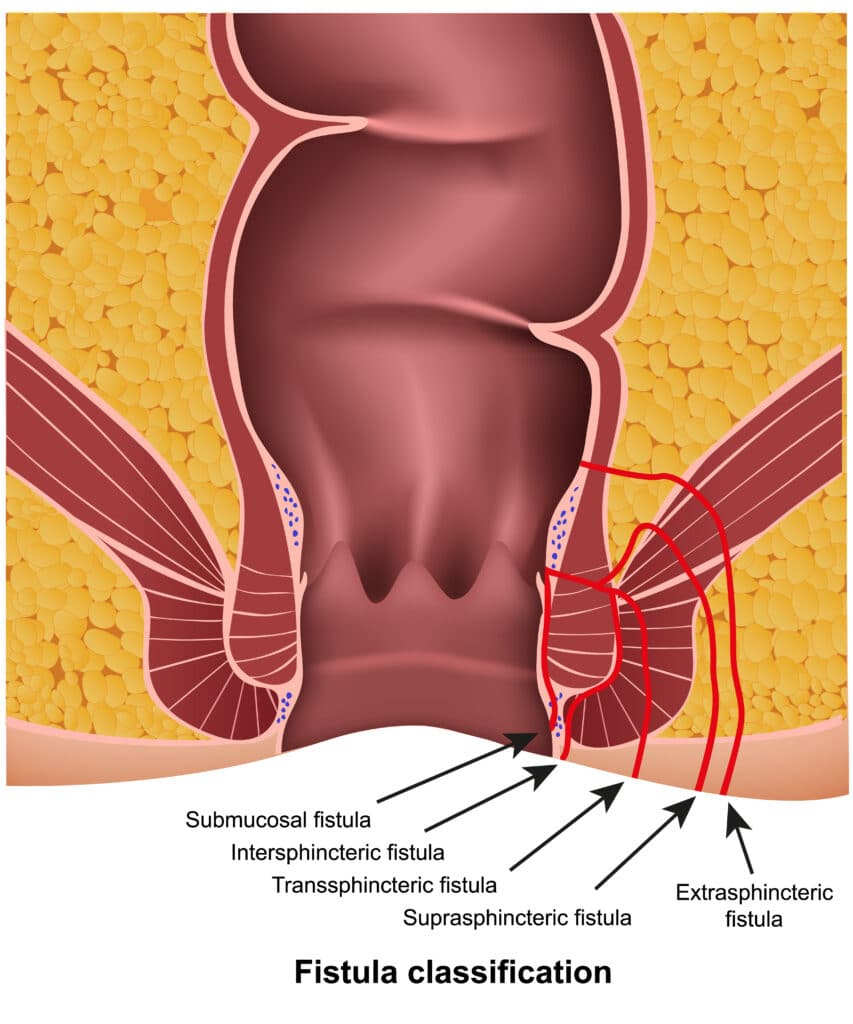
Fistulas are classified by their relationship to parts of the anal sphincter complex (the muscles that allow us to control our stool). They are classified as intersphincteric (going through the inner muscle layer and exiting the skin between the inner and outer muscle layers), transsphincteric (going through both inner and outer muscle layers), suprasphincteric (going through the inner muscle layer and around the outer muscle layer), and extrasphincteric (starting above the anal sphincter and exiting outside the sphincter muscle without going through it). The intersphincteric is the most common and the extrasphincteric is the least common. These classifications are important in helping your surgeon decide what treatment
option is best for you.
Symptoms of an Anal Fistula
Patients with fistulas commonly have a history of a previously drained anal abscess. Anorectal pain, drainage from the perianal skin, irritation of the perianal skin, and sometimes rectal bleeding, can be presenting symptoms of a fistula-in-ano.
How is a fistula diagnosed?
A careful history regarding your symptoms and past medical history are necessary, followed by a physical examination. When diagnosing an anal fistula, an external opening that drains pus, blood or stool is usually seen on examination. Heaped up tissue at the external opening suggests a well-established fistula. A digital rectal exam may produce pus from the external opening. Some fistulas will close spontaneously and the drainage may be intermittent, making them hard to identify at the time of the office visit. A ‘cord’ or tract can be occasionally palpated from the external opening toward the anal canal may help your surgeon locate where an internal opening of the fistula may be inside the anal canal.
Do I need any other tests to diagnose an anal fistula?
Most anal fistulas are diagnosed and managed on the basis of clinical findings. Occasionally, additional studies can assist with the diagnosis or delineation of the fistula tract. Today, both traditional two-dimensional and three-dimensional endoanal ultrasound are a very effective manner of diagnosing and delineating the path of a fistula tract. This may be combined with hydrogen peroxide injection into the fistula tract (via the external opening) to increase accuracy. CT scans can be useful for patients with complicated infections, multiple fistula tracts or with other medical conditions which may present similarly, such as Crohn’s disease. A pelvic MRI has been shown to have accuracy up to 90% for mapping the fistula tract and identifying internal openings.


How is an anal fistula treated?
Currently, there is no medical treatment available for this problem and surgery is almost always necessary to cure an anal fistula. If the fistula is straightforward (involving minimal sphincter muscle), a fistulotomy may be performed. This procedure involves unroofing the tract, thereby connecting the internal opening within the anal canal to the external opening and creating a groove that will heal from the inside out.
Fistulotomy is a long-standing treatment with a high success rate (92-97%). This high success rate must be balanced, however with risk of incontinence (ability to control stool) that comes with division of the anal sphincter muscle. Small amount of muscle can usually be safely divided to treat the anal fistula without compromising continence. Therefore, the surgeon must assess whether a fistulotomy is appropriate for a given patient.
In addition to fistulotomy, there are a number of other surgical treatment options for anal fistula which do not involve division of the sphincter muscles. The two most common procedures utilized in these patients are the endoanal advancement flap and the LIFT procedure. An endoanal advancement flap is a procedure usually reserved for complex fistulas or for patients with an increased potential risk for suffering incontinence from a traditional fistulotomy.
In this procedure, the internal opening of the fistula is covered over by healthy, native tissue in an attempt to close the point of origin of the fistula. Recurrence rates have been reported to be up to 50% of cases. Certain conditions, such as Crohn’s disease, malignancy, radiated tissue and previous attempts at repair, and smoking, increase the likelihood of failure. Although the sphincter muscle is not divided in this procedure, mild to moderate incontinence has still been reported.
Another non-sphincter dividing treatment for anal fistula is the LIFT (ligation of the intersphincteric fistula tract) procedure. This procedure involves division of the fistula tract in the space between the inner and outer layers of your sphincter muscle. This procedure avoids division of the sphincter muscle, and has similar success rate of an endoanal advancement flap.
Most of the operations can be performed on an outpatient basis, but in selected cases, may require hospitalization. Your surgeon at Sacramento Colon & Rectal Surgery Medical Group may discuss multiple options for treatment before your surgery. At the time of surgery, the surgeon does a more thorough exam with you asleep than they can do when you are awake. This may identify characteristics of the anal fistula that may be better treated with one surgical option over the other.
What is a seton?
As mentioned above, if a significant amount of sphincter musculature is involved in the fistula tract, a fistulotomy may not be recommended as the initial procedure. Your surgeon may recommend the initial placement of a draining seton. This is often a thin piece of rubber or suture which is placed through the entire fistula tract and the ends of the seton (or drain) are brought together and secured, thereby forming a ring around the anus involving the fistula tract. The seton may be left in place for 8-12 weeks (or indefinitely in selected cases), with the purpose of providing controlled drainage, thereby allowing all the inflammation to subside and form a solid tract of scar along the fistula tract. This is associated with minimal pain and you can still have normal bowel function with a seton in place. Once all the inflammation has resolved, and a mature tract has formed, one may consider all the various surgical options detailed above as staged procedures.
Treatment of Fistulas in Crohn’s Disease
Fistula-in-ano is very common in Crohn’s disease, which is a chronic inflammatory condition that can affect any part of the gastrointestinal tract. Patients with Crohn’s disease are at increased risk for fecal incontinence because anorectal Crohn’s disease tends to recur and may lead to multiple operations involving the sphincter muscle. It is important to acknowledge that the primary treatment of Crohn’s perianal fistulas is medical, with surgery reserved for treating infection and, occasionally, as a supplement to medical therapy. The treatment should be individualized to the specific patient and incorporate factors that may decrease the potential for fecal incontinence.
What is the recovery like form surgery?
Pain after surgery is controlled with pain medication, fiber, and water. Patients should plan for time at home using sitz baths and avoiding the constipation that can be associated with prescription pain medication. Discuss with your surgeon the specific care and time away from work prior to surgery to prepare yourself for post-operative care.
Can the fistula recur?
Despite proper treatment and apparent complete healing, fistulas can potentially recur, with recurrence rates dependent upon the particular surgical technique utilized. Should similar symptoms arise, suggesting recurrence, it is recommended that you come back to see your physician here at Sacramento Colon & Rectal Surgery Medical Group.