What are anal warts?
Anal warts are caused by HPV infection and are raised growths on the skin and inside of the anus. They can be small or large and cover significant areas of the skin and anal canal. They can be painless but can also cause itching, pain, bleeding, or discharge of mucus. Warts are the easiest way for HPV to transmit to another person but spread can still occur without visible warts.

Are warts cancerous?
Warts can progress to precancer or anal intraepithelial neoplasia (AIN), but AIN can occur from chronic infection without having active warts. AIN is classified as mild (AIN 1), moderate (AIN 2) and severe (AIN 3). The terms HSIL (high grade squamous intraepithelial neoplasia) and LSIL (low grade intraepithelial neoplasia) are also used. It is important to discuss the degree of precancer with your provider and what it means for your care. The different names can get very confusing, and it’s important for you as the patient to understand the diagnosis and the next steps in follow-up and treatment.
AIN can be a skin or internal anal canal lesion that itches, hurts or bleeds, but also may be without any symptoms. Moderate and severe AIN (AIN 2 and 3) is more likely to progress to cancer over time if untreated, especially in high-risk populations.
High risk populations (with increased risk of anal cancer) include HIV positive people, men who have sex with men (MSM), patients where their immune system is suppressed with medications (such as transplant patients) and women with a history of pre-cancer or cancer of the vulva.
Do anal warts always need to be removed?
Yes. If they are not removed, the warts usually grow larger and multiply. Left untreated, warts may lead to an increased risk of anal cancer in the affected area. Fortunately, the risk of anal cancer is still very rare.
Treatment of Anal Warts
External warts can be treated by applying medications or by surgical removal. Topical medicines are not recommended for use inside of the anus, so surgery for internal anal warts is required.
Medications for treatment of external warts can either be chemicals that:
Surgery: There are several ways to surgically remove warts, either in the office or the operating room:
If there are a large number of warts covering wide areas of the skin around the anus or the anal canal, then surgery may be necessary in several stages to prevent scarring of the anus.

Am I cured after my warts are treated?
Warts may come back repeatedly after successful removal. This happens because the HPV virus stays inactive for a period in body tissues. When warts come back, they can usually be treated at your surgeon’s office. If a large number of new warts develop quickly, surgery may be necessary again.
What is anal dysplasia/neoplasia?
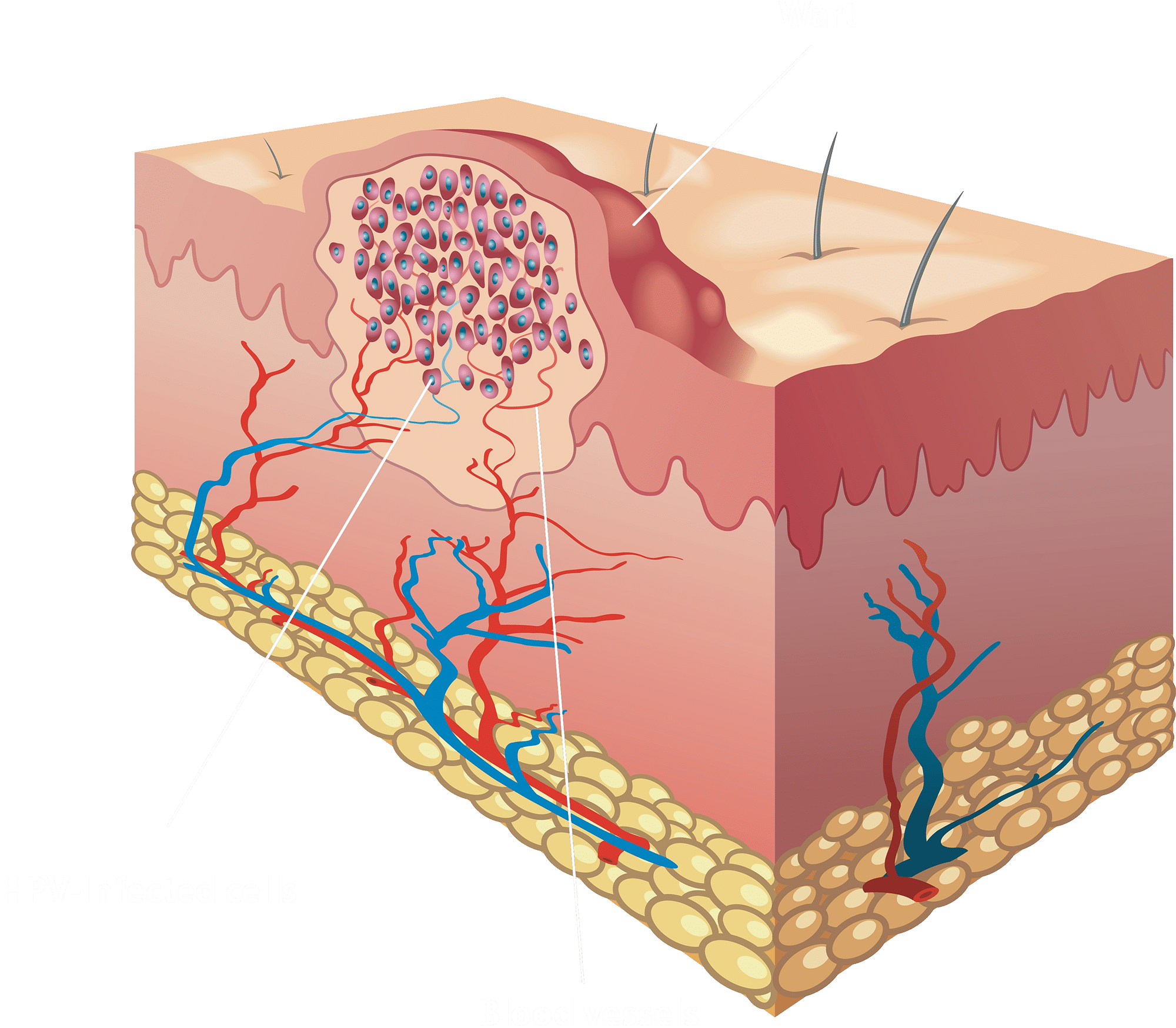
Some warts have abnormal changes seen by the pathologist when they look at the removed wart under the microscope. These changes are called anal dysplasia and can be graded as to how advanced their dysplasia or abnormal changes are under the microscope. These changes are referred to by physicians as low-grade and high-grade anal intraepithelial neoplasia (LGAIN/HGAIN).
Cells that are becoming malignant or “premalignant”, but have not invaded deeper into the skin, are often referred to as HGAIN. While this condition is likely a precursor to anal cancer, this is not anal cancer and is treated differently than anal cancer.
Anal dysplasia (LGAIN/HGAIN) is similar to cervical dysplasia (cervical intraepithelial neoplasia or CIN) in that it originates from a HPV infection and can develop into anal and cervical cancer, respectively. Thus, patients with anal dysplasia need close follow up determined by their physician and any new lesions must be evaluated promptly. A gynecologic examination is also recommended in females, as the presence of HGAIN puts a female patient at risk for having CIN.
Who is at risk for anal dysplasia?
Risk factors for anal dysplasia include:
How is anal dysplasia diagnosed?
Anal dysplasia can be found in anal warts or sometimes these changes are found incidentally at the time of unrelated anal surgery (i.e. hemorrhoid surgery).
Screening procedures available to detect anal dysplasia include anal cytology and high-resolution anoscopy (HRA). However, they are not universally performed and their role in the management of patients with anal dysplasia is unknown at this time.
Anal Papanicolaou (Pap) Smear
Anal Papanicolaou (Pap) smear cytology consists of using anal swabs to sample cells from the anal canal and can be used for both screening patients considered high-risk (see list above) and as follow up after anal dysplasia has been treated. Unfortunately, up to 45% of patients can have a false-positive test by anal PAP for anal dysplasia. As well, it is not known if anal PAP improves your outcome or decreases your risk of anal cancer.
High-Resolution Anoscopy (HRA)
HRA typically involves the application of temporary stains (3% acetic acid and Lugol’s iodine solution) to the anal canal followed by evaluation under high-resolution microscopy to help differentiate normal from abnormal tissue. This is very similar to colposcopy (examination of the cervix) in women who have cervical dysplasia. Directed biopsies are performed for any questionable areas and to identify areas that may need further treatment.
How is anal dysplasia treated?
Anal dysplasia can either be external or internal. Similar to the treatment of warts, both topical medications and surgical excision or destruction of the precancerous tissue are options.
External use of immune boosting medications such as imiquimod and veregen can be used, and a topical chemotherapy agent such as Efudex (5FU) can also applied to treat external dysplasia.
Destruction of internal dysplasia, often using HRA (high resolution anoscopy) can be performed with cautery, using an electric current to destroy focused areas of precancerous tissue. This can be done in the office or the operating room, depending on the extent of the disease.
Careful surveillance of high-grade dysplasia is needed due to a high recurrence rate, and redevelopment of dysplasia over time due to chronic HPV infection.
How should I be followed after treatment for anal dysplasia?
Patients with anal dysplasia should usually be closely followed long term to prevent or detect recurrence, persistence or progression to anal cancer. Physical examinations may be performed at 3 to 6-month intervals. This approach allows for the treatment of recurrent or persistent dysplasia or the detection of anal cancer. Follow-up generally includes digital rectal examination, anoscopic examination, with or without the aid of magnification or the application of acetic acid and Lugol’s solution, and can be performed in an office setting. Anorectal cytology (anal PAP) and/or biopsy may also be included if available in your area. The importance of close follow-up cannot be over emphasized in patients with history of anal dysplasia especially if new lesions develop.